Large Display Replacements / Upgrades by Carrot Medical
Is your medical facility struggling with aging large displays with degraded image quality? Don't let burn-in and other display problems hinder your medical imaging accuracy any longer. Carrot Medical, the pioneer in state-of-the-art medical display technology, has the perfect solution to refresh your imaging environment.
Introducing the Latest in Large Display Technology
If your current large display is struggling to meet the demands of modern medical imaging, it’s time to consider an upgrade. The state-of-the-art C-View Large Display from Carrot Medical is designed to elevate your imaging experience to new heights. With features like built-in protective glass, redundant power supplies, superior LED lighting, improved viewing angles, and superior imaging quality, our displays are engineered to deliver the precision and clarity you need for accurate diagnostics.
Addressing Common Medical Display Problems
Large displays typically have a lifespan of 5 to 7 years, but factors such as equipment misuse and product failure can significantly shorten their longevity. Common issues like cracked screens, dead pixels, image burn-in, and degraded image quality can hinder medical professionals' ability to make accurate diagnoses.
The C-View is the ultimate solution for Cath and EP labs in need of a display upgrade. If your existing large display is showing signs of damage, the C-View offers a premium replacement solution at a surprisingly low price point. Say goodbye to compromised image quality and hello to a superior diagnostic experience.
Top Reasons to Choose Carrot Medical's C-View Large Display:
Cracked Displays? Dead Pixels? Image Burn-In? Degraded Image Quality? No problem! A new C-View eliminates these common issues, ensuring your diagnostic accuracy remains uncompromised.
Vendor-Neutral Compatibility - Carrot Medical's displays seamlessly integrate with major OEM X-Ray systems, including GE, Philips, Siemens, and Canon/Toshiba, ensuring a smooth transition without disrupting your workflow.
Don't let aging large displays hinder your medical imaging capabilities any longer. Upgrade to Carrot Medical's state-of-the-art C-View Large Display and experience a new level of precision, clarity, and accuracy in your medical imaging diagnostics. With solutions designed to address common display issues and seamless integration with major OEM systems, Carrot Medical is the leader in advancing your interventional lab – contact us today!
Renaissance: Maximize Efficiency and Revolutionize Your Lab
Successful procedures in an Interventional Lab are the clear goal of the entire Clinical Team. Other than physician skill -- and patient circumstances -- your greatest chance at optimizing patient outcomes is using the best technology you can to make the procedure as efficient and accurate as possible. This blog post will discuss Carrot Medical’s latest user interface software release (“Renaissance”) for the C-View® Platform -- which enables teams in the Interventional Lab to best use their large screen imaging technology in the most efficient way.
Renaissance is Carrot Medical’s user interface for the C-View Pro and Platinum large display video integrations solutions. Large displays condense multibank screens that show windows such as X-Ray feeds, hemodynamic systems, or mapping into one central display. Large displays are great on their own, but even more effective when used with Renaissance. Renaissance enables the Clinical Team to clearly display the different imaging modalities used during the procedure in the most intuitive way. Providers are given the ability to place and size different windows to their liking; allowing them to prioritize relevant patient information, and improve imaging visibility, thus decreasing case time, and delivering better patient outcomes.
So, what is Renaissance exactly -- and what makes it so great? Let’s narrow it down to three main differentiators.
Easy to Use Interface
While advanced in technology, Renaissance is a very intuitive and easy to use touchscreen interface that remains user friendly. To give a quick overview, there are three sections on the “Preset” page. On the left-hand side, you have User/ Case Type folders. In the middle slot, visuals showing the different displays the user can configure. Then finally, on the far right, the specific layouts the user has saved. This offers great organization as well as visual aids to make the process as intuitive as possible.
Physician Focused
C-View with Renaissance maximizes efficiency in a case through the ability to design and configure layouts exactly to the providers liking. Complete control over presets is essential as everyone has an individual style that best suits them and how they work.
Expanding on the personal presets, physicians and their team can store their unique presets in user folders. These user folders can be renamed to make it easy to find and activate for the specific physician using it at that time.
Real Time Adjustments
At any moment, circumstances of a procedure can change. Renaissance can match these real time changes with on-the-fly adjustments that are easy to make. One can “pinch to zoom” in or out on the touchscreen interface, adjusting the window as best fit. The Clinical Team can also use the auto scaling to quickly achieve pixel perfect inputs by scaling the window to ⅓, 1/2, or full screen on the display. Further, the quick swap tool enables physicians and their team to replace a window quickly with another input. These rapid adjustments to the display can help providers and their team to better visualize key images when they need them.
At the end of the day, physicians want to use cutting edge technology that has a positive impact on patient care. Renaissance is the prime of its kind, with innovative features and a user-friendly interface. Adjustments can be made to the large display on-the-fly, positioning the windows in real time, and in a unique way that best suits the provider at hand. If your goals include optimizing patient outcomes through streamlined workflow solutions and adopting the latest technology to attract and retain physicians, contact us today to learn more about the industry leading Renaissance User Interface and C-View Platform.
Learn more about Renaissance here.
Remote Learning in a Digital World
The world of medicine is driven by improving patient care and continued innovation to find solutions to healthcare issues. It is built upon the pillars of research, education, and practice. Yet, what happens to this process when the ability for experienced physicians to teach less experienced physicians is disrupted?
When experienced physicians no longer have the ability to pass on what they have learned in their career to their students it creates significant issues. It is an issue hospitals and teaching institutions globally have been managing for the past year due to the COVID-19 pandemic. With the rapid spread of the virus, person to person contact has been highly mitigated, and hospitals have reduced their staff and visitors only to those who are essential. Adapting to new regulations to prevent the spread of this deadly virus is a common theme throughout most major institutions. However, what about hospitals and teaching institutions with unpredictable days, and physician and clinical teams that are bound by regulations such as HIPAA? One answer to this complicated situation is the C-Suite Solution from Carrot Medical.
C-Suite is a live-streaming & recording solution that allows users to stream video signals such as ECG, X-Ray, mapping, and more to secure remote locations. This connection from an Interventional Lab to a remote location (such as a classroom or conference room) allows for seamless offsite (socially distanced) learning and teaching. While incredibly useful in normal times, it is extremely important during this pandemic where remote learning has become the norm -- and educators must use alternative methods to educate their students.
Further, C-Suite enables its users to record the clinical team’s audio communication as well during cases to make teaching, reviewing and sharing procedures extremely effective even after the fact. This is a great benefit to have the information you need, when you need it.
Switching to virtual / distanced learning was and is still a must during the COVID-19 pandemic. It would not be a surprise if digitized forms of education became a norm for the future. If this pandemic has shown anything, it has shown that there are always new opportunities to create different learning paths. While remote learning will never fully replace the value of in person education, the flexibility and ease of using digital forms of practice, such as C-Suite, will add meaning to furthering education.
the First U.S. COVID Death: A Heart Attack
On February 29, the first COVID-19 death was reported in the US. For weeks this was considered to be the first coronavirus related casualty on US soil. However, it has been since discovered, that the first COVID related death occurred much earlier, on February 6. The victim, a 57-year-old woman in Santa Clara California, did not die of respiratory problems, as is common to the disease, but rather from a massive heart attack. Without any preexisting coronary heart disease or blot clot issues that could have triggered the attack her death was unexpected. It wasn’t utill later that autopsy revealed that she had traces of COVID-19 in her system. Due to the cause of death not being a commonly associated symptom, and the lack of COVID-19 testing available at the time, her passing was not initially attributed to COVID-19.
An Overlooked Symptom
This first case highlights something important that is being overlooked: How COVID-19 can cause or exacerbate existing heart problems. Since the beginning of the pandemic it has been observed that patients with pre-existing heart conditions are among the most vulnerable groups. New research is suggesting that 1 in 5 patients with COVID-19 have signs of heart injury. This finding is consistent with what has been observed with other respiratory infections. For example, influenza has been known to increase the chances of having a heart attack due to increased inflammation, blood clotting, and blood vessel damage.
Generalized inflammation from COVID-19 is not the only risk to the heart either. Specific organs can also be infected, including the heart itself. When this happens it can cause severe isolated inflammation which can be life threatening. The threat of localized inflammation isn’t just limited to people with preexisting conditions either. It can happen even to anyone regardless of their health prior to becoming infected.
Why aren’t we talking about this?
The link between COVID-19 and heart damage has not gotten much attention. One of the main reasons for this is because COVID-19 causes more respiratory problems than cardiac ones. Another possible cause for this is that heart failure is more of a secondary complication caused by the virus rather than a primary symptom. Furthermore, cardiac injuries are not unique to COVID-19 solely. Other severe viral infections can also cause heart issues. The question is whether the COVID-19 is more virulent toward the heart than other respiratory viruses, which seems to be the case.
There is still much to learn:
COVID-19 is a deadly virus and there is still much we don’t know about it. Understanding how it affects the body is going to help us better manage it and reduce it effects. Understanding this problem better, will lead to lives saved both in this outbreak and other viral outbreaks that may occur. Still, more research is needed to confirm exactly how the coronavirus affects heart function, and which patients with COVID-19 are most at risk for running into heart complications.
The Best X-Ray Systems for Cath and EP Labs
In the Cath lab, time is valuable. The faster the clinical team can diagnose and treat a blockage the better the patient’s outcomes will be. It’s for this reason that the X-Ray is the most critical piece of equipment in the Cath lab. There are 4 main suppliers of X-Ray systems for Cath and EP labs. They are:
GE
Philips
Siemens
Canon
Each has their own perks and quirks, but all are great systems. Here’s an overview of the top 4 systems for Cath and EP labs:
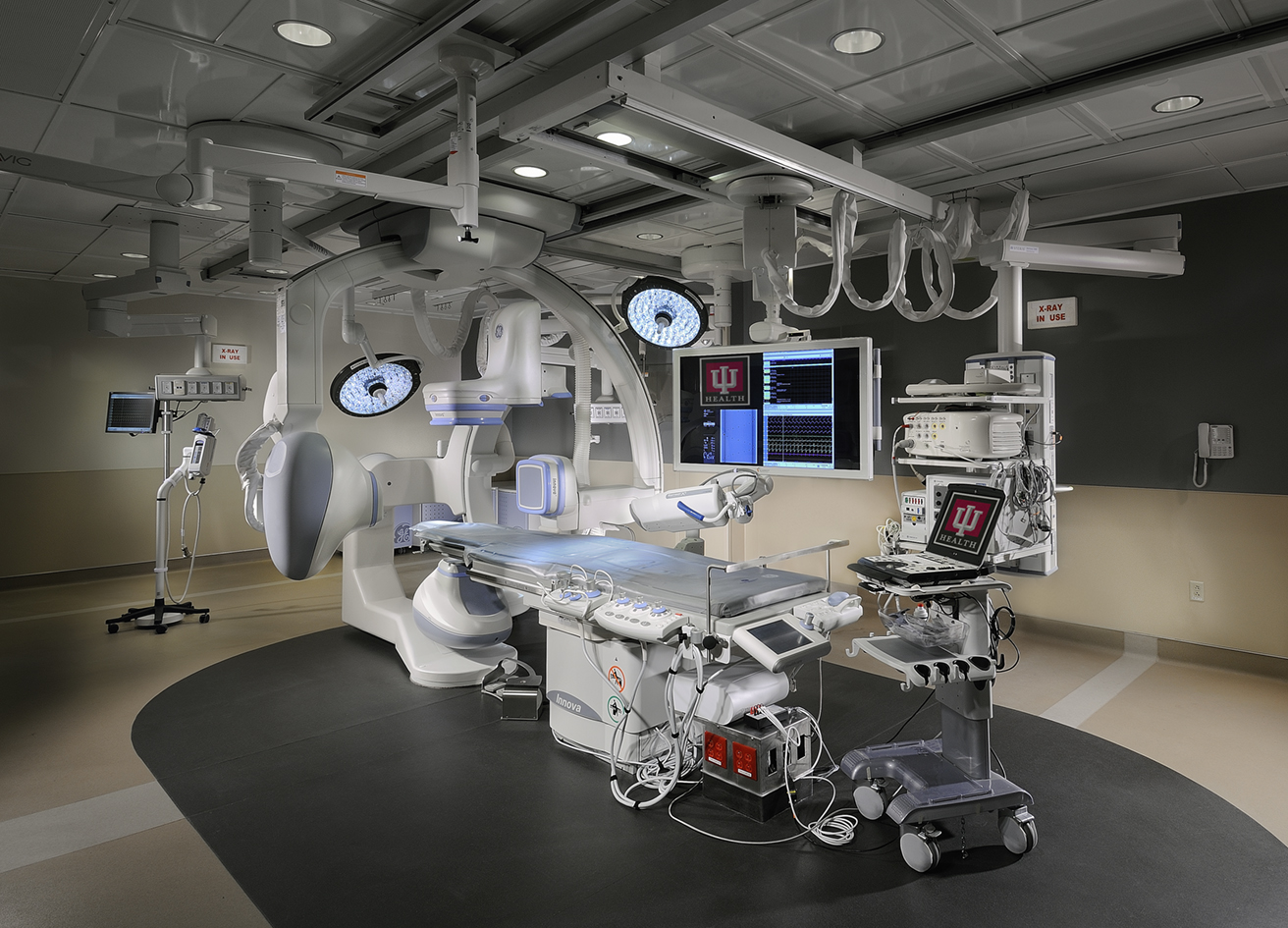
GE Innova IGS 5
The GE Innova IGS 5 is a single plane X-ray system designed with Cath and EP labs in mind. It can be used for oncology and neuro interventions as well. It’s available in various detector configurations:
8.1 inches across
12.2 inches across
16.1 inches across
This flexibility allows hospitals to optimize their labs, as they only need to pay for the size of equipment they need. The offset C-arm is another unique feature, allowing for better access to the patients head for anesthesia and nursing as well as reducing the amount of gantry movement needed to scan from head to groin. The system comes with GE’s proprietary gantry positioning system, known as InnovaSense, which helps move the detector in the optimum position relative to the patient, increasing image quality and reducing radiation exposure.
Philips Azurion 7 C20 & F20
The Philips Azurion 7 series is a single plane X-ray system designed for both non-invasive and open procedures, making it a great fit for hybrid rooms. It features Philips Live Image Guidance systems, such as their StentBoost and EmboGuide, which support clinical workflow and make cases run smoothly. The system comes equipped with a 20” detector, measured from corner to corner.
The system comes with Philips KVM solution, called FlexSpot, allowing for consolidation of the displays in the control room on to one (or two) 27inch display. The Philips Azurion 7 can be mounted on the floor (the F20) or the ceiling (the C20), which is a nice option for labs looking to reduce the footprint of the system.
Siemens Artis zee
The Siemens Artis zee system has 4 configurations: The floor mounted single plane, the ceiling mounted single plane, the ceiling mounted dual plane and the robotic arm mounted single plane zeego. The systems can be configured with one of two detectors:
20 x 20 inch (28 across)
30 x 40 inch (50 across)
The Artis zee ceiling mounted system can hold projection on a particular region during gantry movements using Siemens InFocus and IsoTilt technology. This system is well suited for Cath labs that see a high percentage of peripheral cases due to its full body coverage.
A benefit to robotic arm mounted zeego is that it can be swung up and out of the way when not in use, allowing better access to the patient and optimization of infection control in hybrid operating rooms. The Siemens Artis zee can also be paired with the Stereotaxis NIOBE, allowing for superb guide wire and catheter steering support.
Canon Infinix
The Canon Infinix comes in 7 different configurations, from the budget friendly floor mounted Infinix Core+ all the way up to the Infinix-i 4D CT, which includes a CT scanner. For Cath labs the Infinix-i Core + and the Infinix-i Sky + are both great options, the Core being the floor mounted and the Sky being the ceiling mounted. They are available with the following detector choices:
8 x 8 inch (11” across)
12 x 12 inch (17” across)
12 x 16 inch (20” across)
The Sky + has 210 degrees of mobility and can travel at 80 degrees/sec around the patient, allowing for fast acquisitions that can be used to gather 3D images through digital subtraction angiography (DSA).
Closing Thoughts
Whether you’re constructing a new lab or updating an older lab, these 4 manufacturers all have options that work well. Which you choose will likely depend on what system your medical team is most comfortable with, what price you can negotiate and what features are necessary for your lab. When looking to upgrade an old room it’s worth doing a cost benefit analysis to ensure that upgrading is the most economical solution. Often times we hear hospitals are looking to upgrade because, after a new lab is constructed, the older labs see less use as the doctors prefer the larger display on the new system. In those cases we recommend extending the useful life of the lab via a large video retrofit upgrade, where the multiple monitors are replaced with a large display and the control room monitors are consolidated with a KVM. Doing this retrofit provides much of the benefits of a new system without the price tag of a new x-ray system. For more information about how to advance your interventional lab contact us.
There's an epidemic in the medical field... and no, it's not that nurses are playing cards
“[Nurses] probably play cards a considerable amount of the day” remarked Washington State Senator Maureen Walsh on Monday while arguing against a bill that would require uninterrupted meal and rest breaks for nurses and would protect them from mandatory overtime.
Her comment has garnered significant backlash, including a petition to make her shadow a nurse for a 12 hour shift, now with over 600,000 signatures. Sen. Walsh has since apologized for her statement, but the flow of frustration and anger on social media hasn’t relented. She smacked her hammer against an already cracked dam and is experiencing the repercussions full force.
“[Nurses] probably play cards a considerable amount of the day” remarked Washington State Senator Maureen Walsh on Monday while arguing against a bill that would require uninterrupted meal and rest breaks for nurses and would protect them from mandatory overtime.
Her comment has garnered significant backlash, including a petition to make her shadow a nurse for a 12 hour shift, now with over 600,000 signatures. Sen. Walsh has since apologized for her statement, but the flow of frustration and anger on social media hasn’t relented. She smacked her hammer against an already cracked dam and is experiencing the repercussions full force.
But, the frustration about medical working conditions didn’t begin with her; they have been steeping for many years. Poor working conditions in the medical field is so common that its effects have their own diagnosis: Physician burnout.
Physician burnout is as rampant as it is taboo. Increasing pressures placed on physicians, coupled with the perceived consequences for speaking up, has created a dangerous situation where medical professionals are suffering from the effects of poor working conditions and don’t have a safe place to get help. And, worse still, often the help they do receive isn’t effective. Many hospitals attempt to address the issue with resilience training classes, but these classes may be causing more harm than good. The issue isn’t that health care professionals aren’t tough enough; and taking more time out of their already busy schedules only compounds the problem.
The facts reveal the poor effectiveness of these measures: Male physicians are 40% more likely to commit suicide and female physicians are at a 130% increased risk; resulting in over 400 physician suicides per year. With such a grim statistic it leads you to wonder: Is burnout the correct diagnosis? Many mental health professionals would argue that it is not. Suicide is the symptom of one condition; depression.
Labeling the issue of declining physician mental health as burnout sidesteps the bigger issue: Many medical professionals are suffering from undiagnosed depression. Some balk at that statement, but the facts are clear: Suicide is a symptom of the final stage of depression. Either physicians are suffering from depression or, if they aren’t and are simply burned out, then burnout needs to be treated with the same seriousness that depression is. Regardless of how the issue is labeled the outcome is still the same: Something needs to be done about declining physician mental health. By labeling depression as something that sounds more benign and less dangerous we handicap our ability to solve the issue; it would be in the best interest of medical professionals to just call it what it is and move on with fixing the issue, rather than getting hung up on the particulars.
The unfortunate truth is that mental health diagnoses are, unfortunately, still highly stigmatized and carry a lot of unwarranted baggage, particularly when assigned to people in medicine. Many physicians fear that if they were diagnosed with a mental health issue that they may lose their license or their credibility, perpetuating the problem. Medical professionals are highly trained and well-educated; they are aware of the causes, symptoms and results of depression. The issue isn’t a lack of information but a lack of a solution.
What causes burnout in the medical field?
Stress, when managed in a healthy way, is a good and normal part of life. The bodies natural response to stress helps us perform at our best when it matters most. You know the feeling: Increased heart rate, butterflies in the stomach, muscles tensing ready to act; perhaps you’ve felt it at the start line of a race or when asking someone on a date. This physiological response to fear is a good thing, it helps keep us safe during dangerous circumstances. But stress in unhealthy amounts or when handled improperly can result in lasting damage to the way that the body handles adverse circumstances in the future.
One of the most well-known behavioral studies on stress was performed by Seligman & Maier. They discovered that dogs given shocks without a way to avoid them would, in the future, not attempt to avoid getting shocked, even if the solution was available to them. This research was the foundation for what later has become known as learned helplessness. Learned helplessness is strongly correlated with depression, which intuitively makes sense: When we are upset but feel that we can’t do anything about it we become sad and, when the feelings are chronic, we become depressed.
It’s important to note that learned helplessness has nothing to do with mental strength or fortitude. Physicians are far from weak; to succeed in medical school, complete a residency, and become licensed to practice is no small feat. It’s not the person, it’s the circumstance, that is taking its toll on physician mental health; it’s the repeated exposure to negative stimulus with no agency over the outcome. And it’s this lack of agency that is pushing more and more physicians to a burned-out state; a place where they don’t feel able to help others because they can’t help themselves.
A quarter of US physicians are expected to retire of the next decade and, as the baby boomer generation ages, the amount of people expected to require healthcare is going to rise. The Association of American Medical Colleges projects that we will be short 100,000 physicians by 2030. This imbalance of supply and demand is requiring that healthcare professionals work longer hours and attend to more patients, limiting their ability to provide the best possible care. This in conjunction with an increasing burden of non-critical bureaucratic tasks, declining pay, increasing risk of patient lawsuits, and inefficiencies in medical technology software is wearing medical professionals thin.
What needs to be done?
Resolving the issue of physician burnout is not a simple task, and there are no obvious answers. But, for the safety of healthcare professionals and for the safety of those that they administer care to, we need to find a way to regain what has been lost. We need to recognize that work-induced depression in physicians is a serious issue and that agency over their work environments needs to be restored to them. And, the first steps in restoring this agency to them is by passing laws that protect them and their rights to a safe and healthy work environment.
Intercoms vs. Wireless Headsets for Cath and EP Labs
In the interventional suite having clear communication between the clinical team is critical to the success of the lab. In EP and Cath labs, having a separate control room, procedure room, and supply area can further complicate the matter, increasing the probability of communication related errors. Traditionally, intercom systems have been used to bridge the gap, allowing nurses and technicians in the control room to communicate with the physician performing the case. Another option is to use wireless headsets. So, which solution would fit your lab best? 3 main factors to consider when making a decision about which communication solution to use in your interventional lab are: cost of ownership, ease-of-use, and patient safety.
Cost of Ownership:
Intercoms and wireless headsets both are available in a variety of qualities - and price points. Generally though, an entry level intercom system is more budget friendly than an entry level wireless headset solution. Entry level intercom systems, which is what you find in many labs, work decently well. They usually have a PTT (push-to-talk) mic in the control room and a mic on the boom for the physician, which is always on. If you're on a tight budget, and deciding between a budget friendly intercom system or a cheap headset option, it is best to go with the more durable and more reliable intercom system. Cheap headsets that aren’t designed for medical use can have issues staying connected through leaded glass and generally have poor battery life and low durability, making them an unnecessary risk in the lab.
However, if you are committed to ensuring that your medical team can communicate clearly, a high fidelity intercom system or a medical specific wireless headset system will be your go-to options. Both cost about the same amount up front; so it comes down to preference, warranty terms and install availability. At Carrot Medical we stand behind our products, backing our Pro and Pro Elite wireless headset systems with a 2 and 3 year warranty, respectively. Before you sign the dotted line on any new system, be it intercom or headsets, be sure to read the fine print on your warranty terms and ensure that you are covered adequately. A solid warranty will reduce the cost of ownership long term. Installation is another factor to consider. Because intercoms have to be installed by running cables through the ceiling, a day or two of lab downtime is not uncommon for installation. Headsets are plug-and-play, requiring zero downtime for the lab, and usually only 10-15 minutes to setup and train staff how to use the new system.
Ease of Use:
A communication solution that is too cumbersome or awkward to use won’t last for long; it needs to blend seamlessly into your workflow and allow you and your team to do your jobs effectively. A great communication solution is one you don’t have to think about. Intercom systems are good because they are always setup, don’t have to be charged, and are reliable. But this reliability comes with a cost: Proximity to the mic, background noise and the location of the speaker all affect audio quality, even with high fidelity systems. This can be problematic, especially when you have people moving around the room, or want to be able to exit the lab but stay connected to the case. This inconsistent audio quality, paired with the annoyance of having a loudspeaker magnifying voices and background noise, can make the lab seem chaotic, rather than calm. Wireless headsets solve many of these shortcomings, allowing the medical team to calmly and accurately communicate with one another. Because the microphones are located right next to the speaker’s mouth, rather than feet away, background noise is significantly reduced and the clarity is maintained, regardless of where team members are positioned - inside or outside the lab. The downside of wireless headsets is that a headset must be worn, which some people find a nuisance. For labs that have some physicians that refuse to wear headsets, but still want the benefits of headset systems, a hybrid intercom-headset system can be set up, allowing for both headsets and intercoms to be used at once. However, wireless headsets have come a long way since their inception, and are light weight and comfortable for all-day use.
Patient Safety:
The most important element to consider when looking at a communication system is how will it affect patent safety. The Joint Commission performed a study in 2012 and concluded that “Ineffective hand-off communication is recognized as a critical patient safety problem in health care; in fact, an estimated 80% of serious medical errors involve miscommunication between caregivers during the transfer of patients.”
In the interventional suite it’s crucial there is clear communication between the physician and nurses monitoring the patient. For example, during an ablation, if warning signs aren’t communicated clearly, the catheter could perforate. Another potential issue is that multiple drugs have similar names and miss-hearing this information could be detrimental for a patient’s wellbeing. Wireless headset systems, with close mic proximity, no room-noise feedback, and in-ear audio are the gold standard for high-definition audio in a lab. However, that’s not to say that high fidelity intercom systems don’t work well, because they do, depending on your lab’s setup and requirements.
Final Thoughts:
The decision to go with an intercom system or a wireless headset system for a lab is dependent on a lot of factors: Both have their merits and setbacks to be considered. Cost of ownership, ease-of-use, and effectiveness all weigh on the decision. At Carrot, we hold safety and quality in the highest regard, which is why we recommend either headsets or a headset/intercom hybrid setup, allowing for the utmost clarity between team members and improved safety for patients.
Consider learning more about wireless headset systems click here.
Heart Rate, Heart Health, and How to Train with Heart Rate Zones
We each only have 24 hours in a day and there are many different priorities that levy for that time - Our families, careers, friends, obligations and projects - sometimes our fitness can take a back seat to it all. Recognizing that to maintain a healthy body requires activity is the first step to wellness; and there is a large body of evidence to suggest that this is true. But, regardless of whether we have read the case studies or not, I think we all intuitively know that exercise is good for us; we just don’t know how best to do it or how to make time for it. Once we have decided that making time to exercise is important the next step is deciding how much time to set aside for it and which exercises to do.
A great place to start is with activities that stress your cardiovascular system, ie. cardio. Cardio gets a bad rap, mainly because it’s hard and because the results are a little less external than its more buff cousin, strength training. What makes cardio great though, and why I recommend it before weightlifting, is that it’s very applicable in day-to-day living. Having a healthy cardiovascular system means you can jump longer with your kids on the trampoline, enjoy hiking with your friends more, and outrun the competition in a pickup basketball game. In addition to increasing our enjoyment of daily activities, cardio also burns more calories per hour than weightlifting, meaning you shed weight faster and can fit into those jeans that you haven’t had the heart to give away yet. Speaking of heart; It also strengthens your heart, which is important when you are living in a country where heart disease is the number one cause of death. All this isn’t to say that strength training isn’t necessary, because it certainly is, but cardio is a great place to start when looking to get into shape.
So, we’ve decided that exercise is important, and that we want to start with cardio, but what does that mean? A lot of different activities fall under the umbrella of cardio: running stairs like Rocky, going on a long leisurely hike, running, high intensity interval training (like some Crossfit workouts and Orange Theory), eating cheese on the couch - just checking to see if you’re paying attention! All these are options, but which to choose?
There are 4 Main Types of Cardio
There are 4 main types of cardio. There is all-out, max effort, cardio which occurs during sprints. Then there’s the intensity that is extremely difficult and can only be sustained for 20 minutes to 1 hour (depending on your fitness level). Below that is the intensity that you could maintain for a couple hours, such as hiking or riding a bike. And then last, but not least, is a pace that you could sustain with minimal effort for an extended period of time, like walking. Each of these intensities is correlated with different physiological barriers, which is how we differentiate between the different levels.
Type I: Vo2 Max
The first type we talked about, the-all out effort, is correlated with the measurement of how much air your body can process. At full tilt the limiting factor to your performance is how much oxygen you can get to the cells doing the work. This measurement you may have heard of before, it’s called your V02 max, or more specifically your aerobic capacity. You probably don’t think much about your V02 max except when sprinting in a footrace or running a football into an end zone - and then you become acutely aware of it! Training at this maximum intensity is important if you want to be an elite athlete but, if the other systems in your body aren’t also tuned up to handle running at a sprint, you can risk injury. I wouldn’t recommend incorporating max-effort sprints into your workouts until you have also incorporated weightlifting and stretching, ensuring that your body is ready to handle the increased forces.
Type II: Anaerobic Threshold
The next level of intensity, the one you can sustain for 20-60 minutes, is correlated with your anaerobic threshold. Your anaerobic threshold is the intensity level at which your body is burning more of its glycogen stores than its fat stores (because it’s easier for your body to quickly turn glycogen into energy as opposed to fat). Additionally, at this intensity, your body is unable to evacuate the lactate being produced by your muscles at the rate it is produced, which is why you’ll often hear anaerobic threshold and lactate threshold used interchangeably. If you wanted to know your anaerobic threshold you could go to a sports science clinic and get evaluated (where they put you on a treadmill with a mask over your face to measure your oxygen burn and lactate levels) but, for the most of us, that’s not really necessary. We can determine our own aerobic capacity based on feel. You’ll know when you are at your aerobic threshold because there is a distinct amount of suffering involved: If a 10 was max effort and a 1 is a slow walk, most people find their anaerobic threshold to be around a 7. Not max speed, but at a pace that isn’t sustainable for long and definitely hurts. Exercising at this pace is good, because it can help push our anaerobic ceiling higher, and there is evidence to show that your body’s metabolism is increased after intense workouts, meaning you burn extra calories in the hours following a anaerobic threshold workout, which is pretty cool. If the amount of time you can spend exercising each day is limited to 30 minutes or less then including high-intensity workouts is a good way to make the most of your time. However, for most people, it’s best to incorporate these workouts in maybe once per week (about 10% of your total training volume). I recommend this for two reasons; first, the soreness you feel after these workouts often limits your ability to exercise in the days following and, secondly, because the benefits from longer, easier workouts, is often preferable.
Type II: Aerobic Threshold
The level of intensity below your anaerobic threshold his called your aerobic threshold. Sounds similar to anaerobic, but the difference is that during aerobic exercise your body is performing at a level that allows it to burn both fat and glucose, meaning you can train longer, with less pain, and burn more fat. Your body can only store a limited amount of energy as glucose (glycogen), and once the energy stored in the blood and liver is consumed the body relies on fat to continue operating. Burning through those glycogen reserves usually takes around 2 hours, although it varies from person to person. Once you breach the two-hour mark you really start to make a dent in your fat stores. Burning through those first energy stores slowly is critical to being able to sustain a long effort; otherwise your body will run out of energy faster than it can transition to burning fat stores. This phenomenon goes by many names: hitting the wall, bonking, blowing up… and it’s not a pleasant experience. Maybe you have seen those videos of marathon runners crawling over the finish line because their legs will no longer support them? That’s bonking, and it happens when you train too hard for too long. To avoid this, don’t train at an intensity beyond your aerobic threshold for longer than a couple hours. I recommend that people train mostly at or just below their aerobic threshold, for about 90% of their training, because it gives the best results, isn’t too unpleasant (think of going for a long hike or a couple hour bike ride) and is accessible to everyone (you don’t need a membership to a fancy gym to train at this intensity).
Type IV: Low Intensity
The final level of intensity is that easy, “I-could-do-this-all-day”, type of workout. For people with injuries or older folks that can’t train at a higher intensity, this is the best (and only) way to exercise. But, because most of us don’t have all day to exercise, and want to a good bang for our buck, we’ll skip this one.
Understanding Heart Rate Zones
Okay, so we know we want to do cardio, 90% at aerobic threshold and 10% at anaerobic threshold, a great start. But, how do we know if we are training at the right intensity? There are 2 ways to determine workout intensity. The easiest and cheapest way is by feel: Anaerobic workouts rank around 7/10 on the difficulty scale and aerobic workouts feel about a 3/10. You’ll know if you are at the right intensity based on the duration that you can sustain the intensity as well. Anaerobic should only be sustainable for less than an hour, but longer than 20 minutes and aerobic workouts should be sustainable for many hours, but not easy either. The second, more scientific way to measure our intensity level is by using our heart rate. The rate that our hearts beat at is directly correlated to the amount of stress we are putting on the body (with certain exceptions; an elevated resting heart rate is known as tachycardia). As intensity goes up, so does the heart rate, and thus we can use it to gauge our intensity level. In the olden-days the rule of thumb was to take your age and subtract it from 220 and then do some math to figure out what your heart rate zones were… but c’mon, it’s 2019! We have better methods at our disposal! The “easiest” way to find what your heart rate zones is to get an activity watch that measures heart rate and do a test. And I put easiest in quotes because it’s the easiest way to get an accurate result, but it’s certainly not easy.
The protocol is as follows: Find a flat trail or track that you can run uninterrupted on. Set out at a pace that you can barely sustain for 30 minutes and run as fast as you can for a half hour. It’s not going to be fun, but the harder effort you put in, the better data you will get. Once finished, pull out your phone and find the average heart rate of the last 20 minutes of the run (we discard the first 10 minutes because it takes a while for the heart rate to normalize at this intensity). Then subtract 5% (av. hr x 95%) and you have your anaerobic threshold heart rate. Now, anytime you want to work out at your anaerobic threshold you just run/ bike until the heart rate on your watch matches your calculated anaerobic threshold heart rate. To calculate your aerobic threshold (the intensity that we will use for 90% of our workouts), subtract 30 beats per minute from your anaerobic threshold heart rate and voila; you will have your aerobic threshold heart rate. Knowing this will help you keep your intensity consistent, helping you start at the right pace (it’s a common mistake to start too fast and burn out) and finish strong during those long workouts.
Putting It All Together
The next step, now that you know how to calculate the intensity of your workouts and how to divide your time over these differing intensities, is to determine how much time to spend and how regimented you want to be. The answer to this question is unique for everyone, depending on goals and available time. If your goal is to complete an Ironman distance event, then you will need to set aside a significant amount of time to train and will want a well scheduled and documented training plan. But, if you just want to be healthy and enjoy strenuous activities, then you can afford to be more lax with your training. Regardless of your end goal though, it’s a good rule of thumb to not increase training volume more than 10% each week. Increasing total load more quickly has been shown to result in a higher chance of injury and burnout.
This blog post only scratches the surface of workout intensity levels and exercise planning. To learn more about these topics some helpful resources are The Triathletes Training Bible by Joe Friel (how to train using science), and Finding Ultra by Rich Roll (a memoir about Rich Roll discovering his true potential through endurance sports). My hope is that this article helps you become more educated about sports science, so that you can train smarter, harder and in a way that is enjoyable and fits your lifestyle. Now go lace up those tennies’ and get out there!
6 tips to successfully manage an Interventional lab
Managing an interventional lab is an important task; the degree that a lab is managed well (or poorly) will have a direct impact on the profitability of the lab and, more importantly, the well-being of patients. Below are 6 steps to help you run your interventional lab as efficiently and effectively as possible.
Lead Well
An obvious statement, sure, but an irrevocably true one. A lab (or any organization for that matter) can only succeed to the degree in which it is led. Being a great leader isn't something that can be mastered overnight, but there are some key attributes that we can aspire towards:
Have humility - When we think of what defines a ‘great manager’ or ‘excellent leader’ the characteristics that come to mind are often those of someone who is charismatic, outspoken, and confident. These character traits do indeed make someone standout and attract ‘followers’ but they aren’t necessarily indicative of great leadership. The best leaders have a reserved humility about them. A humble attitude leaves the door open for learning and improvement and allows the people you manage the flexibility to speak openly about their concerns, propelling you and your team to success. Humble leaders aren’t afraid to ask questions, get help, and learn from more experienced people in their network too. “Fake it till you make it” is a recipe for mistakes; being a lifelong learner requires a humble attitude. C. S. Lewis sums it up nicely: “Humility is not thinking less of yourself, it's thinking of yourself less.”
Be a team player - This ties in with the above mentioned point, but it’s worth mentioning. A lab manager who is concerned with exhibiting the dominance of their position and worried about the security of their roll has divided motives and cannot succeed. The best leaders happily pass credit down to their staff while accepting responsibility for the team’s faults as their own. A great book on this topic is Extreme Ownership by Jacko Willink.
Have unflinching determination - In the medical industry there are a hundred different things that can go wrong. When things don’t go to plan your team is going to look to you on how to react. In times of distress, it’s crucial that you stay focused on the end goal. This doesn't mean burying your emotions, but it does mean staying focused on the task at hand, no matter how difficult the circumstances.
Never lose sight of the big picture AND understand each roll - Another crucial function of a leader is to act as the compass during times of confusion or disarray. Having a clear and defined end goal will help you make the right decisions, even under pressure. Often times urgent problems (those that demand your attention right now, like a ringing phone) can continually take precedence over important problems (like thinking about your team’s long-term strategy); being able to distinguish the difference between the two, and delegating the tasks that are urgent but not important, will be crucial to your success. This method of splitting up tasks based on urgency and importance is called the Eisenhower Matrix, named after the President who coined the idea. You can learn more about this method of prioritization here. In addition to keeping your eyes on the big picture you need to be well informed about each roll that every person on your team performs. You don’t need to know how to do every job specifically but, if you don’t understand what it is that each person needs to be doing, you can’t accurately set expectations and hold people accountable to them.
Hire the right people
The US Dept. of Labor estimates the cost of a bad hire to be 30% of their 1st years wage. And that expense only encompasses the sunk costs of bringing on the wrong person. If you keep the wrong person on your team the cost could be significantly worse. So, who are the right people?
Look for attitude first, then skills - You can teach skills, you can’t teach character. Don’t underestimate the negative affect one bad hire can have on the culture of your lab.
Trust your gut - Don’t hire someone you don’t feel 100% confident in. If something doesn’t feel right don’t ignore it. Getting the opinions of others who will be working with the new hire is a great way to vet for culture fit. Another good method to verify fit is to ask yourself the question “Would I want to work for this person?” Asking this will help you see them from the perspective of your current staff and better understand if they are the right person for the job.
Assign rolls well - Give the areas of greatest opportunity to your best performers. It can be tempting to turn your best performers loose on your most problematic tasks, but you must resist doing so. The issue with this approach is that you will miss out on the potential exponential gains to be had with your ripe opportunities and will burn out your talent at the same time. Ask your staff what they are passionate about or what they dream about doing in 10 years. Understanding what makes them light up will help you guide and mentor them, allowing them to reach their fullest potential.
Balance optimism and realism
People tend to error on either one side or other when it comes to optimism and realism. Knowing where your natural tendencies lie will help you be a better lab manager. In the medical field it’s easy to become disconnected from the results of a case because getting too emotionally involved can be draining, particularly if things don’t go to plan. Finding a healthy balance will help you propel your team to success. If you tend to be a dreamer, a creative, an emotional leader - you need to ensure that you aren’t over inflating the outcome of the future based on outcomes in the past. And on the flip side, if you are an analyst, a thinker, a low emotion leader - you need to ensure that you are showing some enthusiasm and excitement about what is to come. Keeping a healthy perspective, one that is neither overly optimistic, nor lacking in zeal, is going to be essential to the success of your lab. A good way to discern where your current tendencies lie is to ask the people who work with you; they will certainly know and that information shouldn’t hurt your feelings, but rather empower you to be a better, more balanced, leader.
Connect you and your team’s passion to the mission
A great manager helps remind people why what they are doing is important. In life it’s easy to get hyper-focused on what is right in front of us and forget why what we’re doing matters. In the medical field there are a myriad of things that can distract you away from the main mission: pinched budgets, staff shortages, difficult patients, threat of malpractice lawsuits, frustrating bureaucracies, lopsided work-life balance… the list goes on. Keeping the bigger picture in mind, for you and your staff, is crucial for the health and success of your lab. There isn’t a one sized fits all answer to this problem; some people respond well to daily meetings to talk about the main objective, some people need time off to recharge and remember why they got into the medical field, some people respond well to writing their thoughts in a journal, and for others speaking their thoughts to someone who can listen and ask good questions is what helps. It’s important as the lab manager that you keep both your heart, and your teams, attached to mission of the lab. Get to know your team and figure out how you can facilitate an environment where they feel connected to the mission. Keeping the team focused on the bigger purpose improves moral and motivation and reduces the risk of burnout and depression. A great read on this topic is Start with Why by Simon Sinek.
Nurture a culture of discipline
A team of people, each thinking critically and making good decisions for the benefit of the team, is more effective than a group of people, each only doing what they are told. This method intuitively makes sense as it maximizes the brain power of the entire group, rather than placing all the thinking responsibility onto the leader, making for a more intelligent, more agile and more productive team. But, in order for this distribution-of-thinking to work, there has to be two things: Autonomy and Discipline. Autonomy (ie. the ability to make decisions without approval) is necessary because without it, regardless of how creative or smart your team is, they won’t be able to enact their ideas. The enemy to autonomy is bureaucracy. Unfortunately, bureaucracy is a dragging anchor behind many otherwise good hospitals. While it can’t be avoided entirely, you can mitigate its affects by creating a culture inside your lab that allows for autonomy, creativity and freedom. Your team will look to you to know whether or not your lab is a safe place to make suggestions and speak openly. You can nurture this autonomous culture by asking open ended questions and getting your teams opinions before making decisions. Also experiment with staying quiet during meetings and assigning people goals without specifically telling them how you want them done.
The second critical ingredient in a successful lab is a culture of discipline. Giving undisciplined people the autonomy to make decisions doesn’t result in success, it results in anarchy and chaos. A balance must be struck where people feel open to express their ideas and take risks, but are also disciplined to stay focused and engaged on the success of the team, not just their ideas. There are many ways to nurture a culture of discipline but one of the most impactful will be seen by who you allow to be on your team (as discussed above in Hire the Right People). By having zero-tolerance for undisciplined team members you communicate to everyone else that you value the culture of the entire group more than the feelings of one person, enforcing the importance of discipline and teamwork. Where a lot of leaders get tripped up when trying to teach and model discipline is when they confuse disciple with perfectionism. Sure, disciplined people make fewer mistakes, but that doesn’t mean they don’t make mistakes. A truly disciplined person, when they do make a mistake, follows procedure, making it known that a mistake was made. Transparency and honesty might be painful at times, because it makes you and your team come face-to-face with your shortcomings, but in the long run it will help make you a better, more highly functioning, team. Nurturing an environment in which professional discipline is paramount means that people can be trusted to make decisions and perform at their best; resulting in less managing and more leading. This balance of autonomy and discipline is an important concept; you can learn more about it in Ray Dalio’s book Principles.
Leverage technology
Over the last couple decades the medical industry has transformed from being largely defined by information to being defined by its technology. Information is still a critical component, to be sure, but now medical information is much easier to access (think online resources like uptodate.com, Sg2, The Advisory Board, ect.). The proliferation of medical information in conjunction with the increasing integration of medical devices into procedures means that it’s becoming ever-more important for lab mangers (and all healthcare providers) to be up-to-date on the latest advancements in technology. The best lab managers are in tune with what the latest technologies are and understand the ROI for the different pieces of equipment available to them. Finances are a limited resource, so allocating them towards the things that will be the most impactful in your lab is important. Don’t be afraid to engage with vendors and ask them about what they see in your workflow. Their exposure to a large number of labs makes them a great resource to learn about what others are doing and can help you make your lab as efficient as possible. Another great way to gather information about what works and what doesn’t is to contact current customers that are already using a particular technology and see how it is affecting the labs performance. Technology is shaping the medical industry; the better we understand how to use it and leverage it, the more successful our labs will be.
Managing a lab is an important job inside a hospital. When it’s done well patients are healthier, residents and physicians are happier and hospitals are more profitable. This blog post was inspired by Jim Collins book Good to Great, check out his book to explore these ideas in more detail.
Medical Display Pricing: How much do they cost?
What is the price of a medical display?
This is one of the first questions we get when discussing a medical display replacement, and we hear it hundreds of times a year. When deciding to upgrade or retrofit a lab, cost is a key factor in the decision-making process.
As you can imagine there are a lot of different variables that affect price, making it difficult to give a one size fits all answer, but this blog post should give you a guideline for what prices to expect.
So, how much do the large displays in Cath Labs, EP Labs and Hybrid Operating Rooms cost?
Most large display integration solutions cost between $100,000 and $200,000, for a turn-key, ready-to-use solution. This price, of course, fluctuates between manufactures and the amount of addons the customer wants. Some example add-ons that customers have to choose between are:
Size: A big screen is more expensive than its smaller counter part
Video Quality: 4K (8mp) is the standard for large medical displays
Amount of inputs: More inputs means more flexibility… and more cost
Installation: Weekend vs weekday
Customization: Special cabling, video routing needs
Just the display:
It’s fairly uncommon for someone to just want just the display, as without the supporting brains (video processor) and control panel (a touch screen tablet), it’s lacking it’s functionality. But, in the event that a display needed to be replaced, the typical cost for a 55 - 58 inch 4k screen is somewhere between $30,000 and $60,000. While these displays might look similar to the one you yell at on Sundays over a bowl of chips (GO HAWKS), there are profound differences between these displays and your TV. To read more check out our article here: What Makes a Medical Display Different than a TV?
The Processor and Controls:
The processor for a medical display system usually costs between $35,000 and $90,000, depending on options. In the past most medical displays were direct video feeds that could only show one image at a time per monitor. However, with the development of large display video integration systems clinical teams can now show multiple video feeds on a single display; these systems are typically controlled by a touchscreen tablet. Using tablets adds a lot of functionality; the most important being that it gives users complete control over the display layout during a case.
Installation:
Installation varies based on the existing equipment and the challenges involved in getting the system in place. You can expect weekday installation to cost somewhere between $5000 to $10,000 while weekend installation ranges from $15,000 to $25,000.
Pricing for other options:
There are other things that need to be brought into consideration when installing a new display.
Swing arms for backup displays cost between $2000 and $5000
Warranties cost between $20,000 and $25,000 a year
The numbers are broad, but I hope it gives you a reference of what to expect when looking for a new medical grade display. Wondering if you should keep your old equipment and get a new display, or if it’s time to get all new equipment? Read our article: When to Retrofit and when to re-equip your EP lab or Hybrid OR.
Looking to upgrade your lab? Contact us for a quote.
Medical Display's vs. TV
What’s the difference between a medical display and a TV?
At face value, medical displays and TV’s look very similar. They can have the same resolution and be the same size, so what’s the difference? Despite that fact that they look the same, the size and resolution is about where the similarities stop. Why is that?
3 Letters: FDA
In 1906 the Food and Drug Administration was formed to protect and promote public health (Also, in 1906, the football rules committee legalized the forward pass!) While the FDA’s domain includes, as you would expect, food and pharmaceutical regulation it also branches into other areas of public health, including healthcare. Fast forward to 1976, after multiple deaths and infertility caused by a contraceptive device (Dalkon Shield), the Food-Drug-and-Cosmetics-Act was amended to include regulation and review of medical devices with the intent of providing the public reasonable assurances of safe and effective devices.
The FDA classifies medical devices under 3 different categories based on the risk they pose to patients:
Class I: These devices pose the lowest risk and include things like tongue depressors (does that make you gag just hearing it?), bandages and crutches.
Class II: These devices pose an intermediate risk and include things such as electrocardiographs, hearing aids and, yes, displays used in operations.
Class III: These medical devices pose the greatest risk to patient health and include things such as implantable pacemakers, stents, and heart valves.
Medical displays, being a class II device, have to go through a testing process, known as the 510(k), with the FDA before they are cleared for market. If you do a little digging you will notice that some devices are ‘cleared for use’ by the FDA and some are ‘approved’ by the FDA, in which case I would applaud you for your attention to detail. When the FDA uses the 510(k) process to review a product they deem it cleared. When they use the premarket approval process (also known as PMA) then they say it was approved. The less stringent 510(k) approval process is used for class II devices and the more thorough PMA process is used for class III devices. Only about 1% of medical devices are screened via the PMA process.
Because of the standards imposed by the FDA, medical screens have to be built in a way that ensures patient safety, whereas TV’s don’t have to adhere to the same standards. Below are some of the distinguishing factors between your TV at home and a display in a hospital.
How they’re different:
Reliability: If your TV burns out in the 4th quarter of a game that’s a bummer. If a medical display being used in an operation stops working, it’s a massive problem. Additionally, even slight problems, like a burned-out pixel, could lead to an incorrect assessment in the lab, where at home you wouldn’t even notice it. Medical displays are built to be more reliable than their consumer counter parts.
Brightness: Known in the industry as luminance, the brightness of a display affects the physician’s ability to see all the details clearly. This effect is magnified when the screen is being viewed at an angle, as a brighter screen is required to see the same level of detail when you aren’t facing the screen head-on. Medical displays are brighter than their consumer counter parts and are designed to be more resistant to fade over time. The brightness setting is also fixed, ensuring that physicians are making consistent and accurate assessments.
Color Depth: Distinguishing colors, and interpreting greyscale images is very important for physicians. Medical displays distinguish colors and shades from another in a uniform and accurate manner, allowing for correct analysis in the lab.
Durability: Medical displays are built to withstand a lot more abuse. They have stronger frames, sometimes metal, and thick plexiglass protection on the front. They also need to be easily cleaned and sterilized and cannot contain materials that could harbor pathogens.
Use-Specific Features: In addition to the quality of the display, many medical screens have built in specific-use features. Some have handles around the edges so that they can be pushed and pulled easily when mounted on a swing arm. Also, some have the ability to receive multiple inputs so that they can display multiple different inputs all at once.
So, when can I use a consumer display in a medical setting?
These types of decisions are best left to the Biomedical Engineers at hospitals, but generally a consumer grade display is fine for any application that a failure wouldn’t risk the quality of care a patient receives. You will find consumer grade screens in control rooms, at front desks, and at other workstations.
Looking for a high-quality medical display for your interventional lab? We make some of the best in the industry: Lets talk!
When to Retrofit and when to Replace your Interventional Lab Equipment
Everyday technology is affecting how healthcare professionals interact with patients. Gone are the days of analog data on spools of paper (well mostly gone anyways); everything is going digital and advancing at a rapid rate. This is excellent for patients as they are able to receive the highest quality of care.
But all this growth isn’t without its challenges. The main one being: How do healthcare providers keep up?
There is a constant inflow of new information; fascinating studies containing updated data are emerging weekly. Keeping up to date on newly published scientific articles is a lot of work as it is; add on the burden of keeping up with new technology and it can feel overwhelming. With new equipment constantly being produced it causes you to wonder: when should you upgrade the technology in your lab?! The major OEM’s will tell you to upgrade frequently, but of course they will, they have a vested interest in the amount of new medical devices that are purchased. So, what’s the truth?
The Fundamental Issue with Aging Equipment
The main problem with aging equipment is that it ages at different rates: The relevancy of old medical equipment varies. Some medical devices haven’t changed in decades and are just repackaged to look new. Yet, other medical devices are rapidly changing, being fundamentally redesigned every couple of years as new data and techniques emerge. This creates a situation where a 10-year-old lab will have equipment that works flawlessly and doesn’t need to be replaced, but will also have devices that are hopelessly outdated.
Managing Outdated Equipment
Often times with medical equipment the interface, displays, and data management tools all age much faster than the actual equipment does (such as x-rays, hemodynamic systems, etc.). Many of our everyday use items age in the same way. Cameras are one example: Lenses, as long as they are kept clean and free of dust and scratches, are good for decades. It’s not uncommon for lenses to gain value over time, rather than depreciate, as they don’t lose their usefulness with age. Contrast that with the body of the camera, the part that contains the sensor and the interface. The body of a camera loses value at a dismal rate because this part of the equipment system changes at a more rapid rate. Medical equipment depreciates in a similar way: The imaging equipment remains relevant but the monitors and display equipment ages quickly.
What are lab managers to do?
A clever way to save money and keep your lab up to snuff is to replace displays, or other components that have aged quickly. This budget friendly option allows you to give your patients the best quality care without requiring you update everything. The C-View system from Carrot is one example of this upgrade-don’t-replace mentality. The C-View platform replaces a multi-bank setup of old CRT screens with one 4k display, allowing physicians to customize what is on the large display at any moment, making their job easier and decreasing case time. This economical solution allows physicians to have the tools they need at a price point that fits most budgets.
The key to staying above water in today’s rapidly changing medical environment is to focus resources on areas that will give the highest return on investment. Analyzing what needs to be replaced and what can be retrofitted will maximize capital dollars when investing in an interventional lab. For more information about equipment retrofit options, contact us.